Background: CD19-targeted chimeric antigen receptor T-cell therapies (CART) have remarkable overall response rates (ORR) for relapsed/refractory diffuse large B cell lymphoma (DLBCL). Given the time interval between apheresis (Aph) and product delivery, bridging interventions (BI) have been used to provide disease control prior to CART infusion. Real world data suggests about half of patients (pts) require BI such as systemic therapies (ST), radiotherapy (RT) or combined modality therapy (CMT). Early data has associated BI with poorer prognosis however this remains unclear. While no BI strategy has emerged as superior, there is strong rationale to use RT including rapid palliation and cytoreduction with potential immune augmentation. We reviewed BI experience at a comprehensive cancer center.
Methods: We analyzed pts who received commercial CART between 2/2018-9/2019. Pts were stratified by BI category including no BI (NBI), ST (any chemoimmunotherapy, targeted agent and/or steroid post Aph), RT (3 months pre-Aph up until CART infusion) or CMT (both ST and RT). Characteristics, toxicities and outcomes were analyzed overall and for 3 subgroups: 1) NBI, 2) ST and 3) RT+CMT. Response assessment was by PET per Lugano Criteria. Progression free survival (PFS) and overall survival (OS) were analyzed from day of CART infusion using Kaplan Meier and univariable proportional hazards.
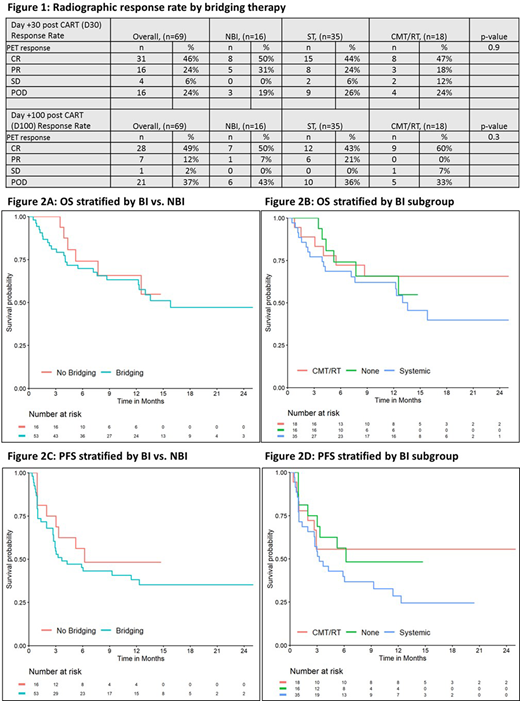
Results: Overall, 69 pts (70% male, median age 64) with 97% DLBCL (41% transformed indolent) received CART. At Aph, 67% were advanced stage and 38% had >1 bulky site (>7.5cm). Pts received axicabtagene ciloleucel (axi-cel, 68%) or tisagenlecleucel (tisa-cel, 32%) following lymphodepletion (LD) with median Aph to infusion time of 35d (range 20-77). Most (77%) received BI, specifically ST (n=35, 51%), RT (n=11, 16%) or CMT (n=7, 10%). Compared to NBI (n=16), +BI pts were less likely to be post autologous transplant (p=0.05), more likely to have osseous disease (p=0.02), and trended to greater median LDH at Aph (NBI: 214 u/L, ST: 301, RT+CMT: 272, p=0.08). Other factors were similar across BI/NBI groups including performance status, cell of origin, share of axi-cel/tisa-cel, pre-CART stage and bulky/extranodal disease.
Median hospital stay was 17d and 25% required ICU; both did not vary by BI (p>0.9 and p=0.4, respectively). Rates of cytokine release syndrome (CRS) also did not vary (NBI: 88%, ST: 77%, RT+CMT: 83%, p=0.7). Of 56 total CRS cases, 7 (13%) were grade 3+ and all occurred in +BI pts (ST: n=4/27, 15%; RT+CMT: n=3/15, 20%, p=0.3). Overall rates of immune effector cell-associated neurotoxicity syndrome (ICANS) were 39% and did not differ by BI status (p=0.4). Rates of grade 3+ ICANS were NBI: 1/6 (17%), ST: 9/16 (56%), RT+CMT: 4/5 (80%), p=0.11. Median duration of ICANS was longer for NBI (7.0d) vs. ST (4.5) or RT+CMT (4.0), p=0.04. Tocilizumab and steroid use rates were 45% and 41%, respectively and did not differ by BI (p=0.2, p=0.8).
ORR was similar irrespective of BI status (Fig 1A). With median follow-up of 13.5m, there were 30 deaths and median OS was 15.8m. Compared to NBI, +BI did not have significantly worse OS (hazard ratio, HR=1.2, 95%CI: 0.5-3.0, p=0.7, Fig 2A). By BI status, 12m OS is NBI: 66% (95%CI: 45-96%), ST: 62% (48-81%) and RT+CMT: 66% (47-92%) (Fig 2B). Significant predictors of poorer OS are presence of bulk (HR 4.0, p<0.001) and elevated LDH at Aph (HR 2.7, p=0.01). Compared to NBI, +BI pts had nominally, but non-significantly poorer PFS (HR 1.4, 95%CI: 0.7-3.1, p=0.4, Fig 2C). Though limited by sample size, early data suggests ST (6m PFS: 40%, 95%CI: 26-60%) might have inferior PFS to NBI (6m PFS: 56%, 95%CI: 37-87%) or RT+CMT bridging (6m PFS: 56%, 95%CI: 37-84%) (Fig 2D). Presence of >1 bulky site at Aph was also associated with poorer PFS (HR 2.6, p=0.003).
Conclusions: Bridging therapies are increasingly used prior to CART infusion and were utilized for >75% of this cohort. This exceeds benchmarks and may reflect a uniquely urgent population or impact of tisa-cel utilization with more baseline bridging at our referral center. Acknowledging the limitation of a small NBI comparator subgroup, we find BI to be safe and not associated with worse toxicity or outcomes. Early data suggest that RT or CMT may be a preferable BI strategy compared to ST though larger cohorts are needed for validation and to clarify the unique impact of RT without ST. More intensive cytoreductive strategies might be beneficial for bulky disease pre-CART.
Perales:Celgene: Honoraria; Nektar Therapeutics: Honoraria, Membership on an entity's Board of Directors or advisory committees; Merck: Consultancy, Honoraria; Miltenyi Biotec: Research Funding; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees; Cidara Therapeutics: Other; Servier: Membership on an entity's Board of Directors or advisory committees, Other; NexImmune: Membership on an entity's Board of Directors or advisory committees; Medigene: Membership on an entity's Board of Directors or advisory committees, Other; Omeros: Honoraria, Membership on an entity's Board of Directors or advisory committees; MolMed: Membership on an entity's Board of Directors or advisory committees; Incyte Corporation: Honoraria, Research Funding; Bristol Myers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees; Bellicum: Honoraria, Membership on an entity's Board of Directors or advisory committees; Abbvie: Honoraria, Membership on an entity's Board of Directors or advisory committees; Kite/Gilead: Honoraria, Research Funding. Batlevi:Life Sci, GLG, Juno/Celgene, Seattle Genetics, Kite: Consultancy; Janssen, Novartis, Epizyme, Xynomics, Bayer, Autolus, Roche/Genentech: Research Funding. Dahi:Kite: Consultancy. Park:Artiva: Membership on an entity's Board of Directors or advisory committees; Genentech/Roche: Research Funding; Novartis: Consultancy; Fate Therapeutics: Research Funding; Servier: Consultancy, Research Funding; Juno Therapeutics: Research Funding; Kite: Consultancy, Research Funding; Incyte: Consultancy, Research Funding; GSK: Consultancy; Autolus: Consultancy, Research Funding; Intellia: Consultancy; Minverva: Consultancy; AstraZeneca: Consultancy; Allogene: Consultancy; Takeda: Consultancy, Research Funding; Amgen: Consultancy, Research Funding. Scordo:Kite - A Gilead Company: Other: Ad-hoc advisory board; Omeros Corporation: Consultancy; Angiocrine Bioscience, Inc.: Consultancy, Research Funding; McKinsey & Company: Consultancy. Shah:Janssen Pharmaceutica: Research Funding; Amgen: Research Funding. Giralt:CELGENE: Consultancy, Honoraria, Research Funding; OMEROS: Consultancy, Honoraria; NOVARTIS: Consultancy, Honoraria, Research Funding; KITE: Consultancy; MILTENYI: Consultancy, Research Funding; ACTINUUM: Consultancy, Research Funding; TAKEDA: Research Funding; JAZZ: Consultancy, Honoraria; AMGEN: Consultancy, Research Funding. Sauter:Genmab: Consultancy; Bristol-Myers Squibb: Research Funding; GSK: Consultancy; Gamida Cell: Consultancy; Celgene: Consultancy, Research Funding; Kite - a Gilead Company: Consultancy; Precision Biosciences: Consultancy, Research Funding; Spectrum Pharamaceuticals: Consultancy; Novartis: Consultancy; Sanofi-Genzyme: Consultancy, Research Funding; Juno Therapeutics: Consultancy, Research Funding. Palomba:Genentech: Research Funding; Juno Therapeutics, a Bristol-Meyers Squibb Company: Honoraria, Research Funding; Pharmacyclics: Honoraria; Merck: Honoraria; Celgene: Honoraria; Novartis: Honoraria; Regeneron: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal